Introduction to Thalassemia
Thalassemias are a heterogeneous group of genetically determined hemolytic anemias due to an impaired synthesis of globin chains which are an integral part of the hemoglobin molecule. Originally diagnosed in Greece, the disease was named thalassemia (the sea) because of the geographical location of Greece along the Mediterranean Sea since its original discovery; the disease has been found to be prevalent in the Mediterranean countries, in the Middle East, the Indo-Pak subcontinent and the South-East Asian countries. This stretch of land is collectively called the thalassemia belt. With rapid migration of the population across the globe and the world transforming into a global village, the concept of ‘thalassemia belt’ is giving way to globalization of thalassemias.
Only forty years ago Thalassaemia was considered to be non-entity.
Epidemiology of thalassemia:
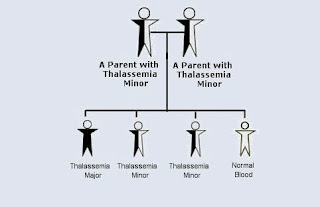
In Pakistan it is the β-thalassemia which is the most prevalent, other forms of thalassemias like α-thalassemia and β-thalassemia and hereditary persistence of fetal hemoglobin are extremely uncommon. Gene frequency of β-thalassemia in Pakistan stands at 6% With a population of 140 millions, there are over 8 million carriers of β-thalassemia gene Inter-marriages and first cousin marriages has resulted in a high incidence of homozygous β-thalassemia (β-thalassemia major). It is estimated that in Pakistan at present there are about 121,000 patients of b-thalassemia major. Since Thalassaemia is the single most common genetic disorder in Pakistan, it is important for the health care providers to be fully conversant with the inheritance patterns of the disease, the laboratory procedure which establish the diagnosis and the counseling techniques to prevent the transmission of this disease in homozygous state damaging to the functional integrity of the cell red cell membrane. This causes severe hemolytic anemia in the fetus, marked hepato-splenomegaly, marked cardio megaly, severe anemia, edema and heart failure resulting in intra-uterine death of the foctus.
Laboratory Investigations:
There are three sets of investigations which are commonly done partly to study the pathological changes in the body and partly to establish the diagnosis. There include hematological, biochemical and radiological investigations. It must be emphasized at this juncture that not all investigation need be carried out in all types of thalassemia. This point is highlighted in the clinical manifestations of thalassemias.
1. Hematological:
These include complete blood count including a critical morphological review of the blood smear (and bone marrow when indicated) Hemoglobin. Electrophoresis on cellulose acetate establishes the diagnosis in all types of thalassemia. Supravital stains are done for the demonstration of reticulocytes and Hb H inclusions as and when indicated.
2. Biochemical:
Biochemical investigation commonly include the estimation of serum bilirubin serum LDH and serum iron profile (serum iron, serum Transferrin or T/BC and serum ferritin) The usual serum iron profile in Thalassaemia syndromes is listed below.
Thalassemias are a heterogeneous group of genetically determined hemolytic anemias due to an impaired synthesis of globin chains which are an integral part of the hemoglobin molecule. Originally diagnosed in Greece, the disease was named thalassemia (the sea) because of the geographical location of Greece along the Mediterranean Sea since its original discovery; the disease has been found to be prevalent in the Mediterranean countries, in the Middle East, the Indo-Pak subcontinent and the South-East Asian countries. This stretch of land is collectively called the thalassemia belt. With rapid migration of the population across the globe and the world transforming into a global village, the concept of ‘thalassemia belt’ is giving way to globalization of thalassemias.
Only forty years ago Thalassaemia was considered to be non-entity.
Epidemiology of thalassemia:
In Pakistan it is the β-thalassemia which is the most prevalent, other forms of thalassemias like α-thalassemia and β-thalassemia and hereditary persistence of fetal hemoglobin are extremely uncommon. Gene frequency of β-thalassemia in Pakistan stands at 6% With a population of 140 millions, there are over 8 million carriers of β-thalassemia gene Inter-marriages and first cousin marriages has resulted in a high incidence of homozygous β-thalassemia (β-thalassemia major). It is estimated that in Pakistan at present there are about 121,000 patients of b-thalassemia major. Since Thalassaemia is the single most common genetic disorder in Pakistan, it is important for the health care providers to be fully conversant with the inheritance patterns of the disease, the laboratory procedure which establish the diagnosis and the counseling techniques to prevent the transmission of this disease in homozygous state damaging to the functional integrity of the cell red cell membrane. This causes severe hemolytic anemia in the fetus, marked hepato-splenomegaly, marked cardio megaly, severe anemia, edema and heart failure resulting in intra-uterine death of the foctus.
Laboratory Investigations:
There are three sets of investigations which are commonly done partly to study the pathological changes in the body and partly to establish the diagnosis. There include hematological, biochemical and radiological investigations. It must be emphasized at this juncture that not all investigation need be carried out in all types of thalassemia. This point is highlighted in the clinical manifestations of thalassemias.
1. Hematological:
These include complete blood count including a critical morphological review of the blood smear (and bone marrow when indicated) Hemoglobin. Electrophoresis on cellulose acetate establishes the diagnosis in all types of thalassemia. Supravital stains are done for the demonstration of reticulocytes and Hb H inclusions as and when indicated.
2. Biochemical:
Biochemical investigation commonly include the estimation of serum bilirubin serum LDH and serum iron profile (serum iron, serum Transferrin or T/BC and serum ferritin) The usual serum iron profile in Thalassaemia syndromes is listed below.
- Serum iron Increased
- TIBC Normal
- % transferrin saturation is Increased
- Serum Ferritin Increased
Clinical Features:Clinical features of thalassemias manifest a wide spectrum. one the one hand there is the α-thalassemia minima which cannot be diagnosed except through family studies. At the other end of the spectrum there is a-thalassemia major which is inconsistent with intra uterine existence. It is called hy drops fetal is or Hb Barts disease. In this condition the baby is either born dead or he dies soon after birth In between these two extremes there are a-thalassemia heterozygous b-thalassemia heterozygous Hb H disease, (b-thalassemia major).
Symptoms are chiefly due to anemia and the cardiovascular compensatory mechanisms hemolysis process and hematopoietic compensation are reflected in hepatosplenomegaly consequent upon intramedullary hematopoietic ( or myeloid metaplasia ).
Another set of symptoms are due to iron overload consequent upon increased iron absorption from GIT and repeated blood transfusions which are necessary to sustain patients with b-thalassemia major.
α-thalassemia minima:
In this condition 75% of the a-genes are intact and functional. The amount of hemoglobin produced is normal and there are no clinical or laboratory parameters to even suspect the presence a-thalassemia. The disease comes to light only as a result of gene studies in the family.
α-thalassemia minor:
In this condition two out of four a-gene are intact and functional hemoglobin synthesis is reduced (but not by 50% as expected because of the loss hypo chronic in type with reticulocytes and mild unconjugated hyperbibribnema. There is no splenomegaly or Hepatomegaly nor is there any increased incidence of liver disease, gall stones or leg ulcers. Hematological abnormalities show mild degree of Microcytic and hypo chronic anemia supra vital stain using BC B stain for show a rare red cell which contains Hb H inclusions.
Hb H disease:
This condition results from loss of 3 functional α-genes, there is moderately severe degree of Microcytic and hypochromic and reticulocylosis Supra-vital stain shows large number of red cells which contain many Hb H inclusions. These patients do slow features of chronic anemia although they are usually not transfusion dependent a-thalassemia major (Hb Bart disease). In this condition all α-genes are absent the only globin chains in these red cell are γ-chains (Gamma chains). Their polymerizations into tetramers produce Hb Bart (g4)..
Symptoms are chiefly due to anemia and the cardiovascular compensatory mechanisms hemolysis process and hematopoietic compensation are reflected in hepatosplenomegaly consequent upon intramedullary hematopoietic ( or myeloid metaplasia ).
Another set of symptoms are due to iron overload consequent upon increased iron absorption from GIT and repeated blood transfusions which are necessary to sustain patients with b-thalassemia major.
α-thalassemia minima:
In this condition 75% of the a-genes are intact and functional. The amount of hemoglobin produced is normal and there are no clinical or laboratory parameters to even suspect the presence a-thalassemia. The disease comes to light only as a result of gene studies in the family.
α-thalassemia minor:
In this condition two out of four a-gene are intact and functional hemoglobin synthesis is reduced (but not by 50% as expected because of the loss hypo chronic in type with reticulocytes and mild unconjugated hyperbibribnema. There is no splenomegaly or Hepatomegaly nor is there any increased incidence of liver disease, gall stones or leg ulcers. Hematological abnormalities show mild degree of Microcytic and hypo chronic anemia supra vital stain using BC B stain for show a rare red cell which contains Hb H inclusions.
Hb H disease:
This condition results from loss of 3 functional α-genes, there is moderately severe degree of Microcytic and hypochromic and reticulocylosis Supra-vital stain shows large number of red cells which contain many Hb H inclusions. These patients do slow features of chronic anemia although they are usually not transfusion dependent a-thalassemia major (Hb Bart disease). In this condition all α-genes are absent the only globin chains in these red cell are γ-chains (Gamma chains). Their polymerizations into tetramers produce Hb Bart (g4)..

Very Informative. Thank you so much
ReplyDelete