A glance at Beta Thalassemia minor
Age : 24 Sex: Female Occupation: Housewife
NUMERICAL VALUES
Beta – Thalassaemia Minor
Beta-thalassemia minor is a genetic disorder which shows strong geographical predilection. It is mostly encountered along the Mediterranean belt, the Arabian Peninsula and the Indo-Pak subcontinent. In Pakistan the frequency of beta-thalassemia gene is nearly 6 %. It is therefore not uncommon to come across these patients in clinical practice. A systematic analysis of the hemogram highlights the following features.
NUMERICAL:
Hemoglobin and hematocrit are both decreased. An unexpected finding is a high red cell count. In addition, the reticulocyte count is also increased. Total leukocyte count, platelet count and ESR are within normal limits.
RED CELL INDICES:
MCV and MCH are significantly decreased while MCHC% is nearly normal. This is at variance with the expected value of MCHC% which is decreased in almost all instances where MCV and MCH are below normal as exemplified by iron deficiency anemia. Red cells are microcytic and hypochromic hence anemia is of microcytic and hypochromic type.
DIFFERENTIAL LEUKOCYTE COUNT:
There is no deviation from the norm in the percentage values of different types of white cells. No abnormal leukocytes are seen.
MORPHOLOGY:
As expected, the morphology of the peripheral blood smear is quite revealing. The abnormalities are confined almost entirely to the red cell series. There is some variation in the size and shape of the red cells which, in conformity with the red cell indices, are predominantly microcytic and ‘hypochromic’. In addition some fragmented red cells, pencil cells and micro-spherocytes are also seen. A prominent feature is the presence of target cells and stippled red cells (basophilic stippling). There is also some variation in the color of the erythrocytes. Many hypochromic, some normochromic, a few polychromatophilic and occasional brightly stained red cells are present. This tinctorial heterogeneity is called anisochromia or anisochromasia.
Polychromatophilic erythrocytes are a shade larger than the normochromic red cells and on reticulocyte stain they display the characteristic reticulum in their cytoplasm. Polychromasia on Romanowsky’s stains (Wright’s, Leishman’s or Giemsa’s stain) is the counterpart of the reticulocytes on reticulocyte stain ; the greater the polychromasia, the higher the reticulocyte count.
Microcytic and hypochromic red cells are seen in a number of conditions; these are listed below.
• Iron deficiency anemia
• Thalassaemia syndromes
• Hemoglobinopathies
• Sideroblastic anemias
• Chronic lead toxicity
• Chronic renal failure
• Chronic infections
Of these disorders, iron deficiency anemia and Thalassaemia syndromes account for almost 90% of the cases of significant microcytosis and hypochromia (MCV less than 70 fl and MCH less than 25 pg).
A detailed history and a thorough physical examination coupled with socio-economic, obstetric and family history can help identify these two conditions in a vast majority of cases.
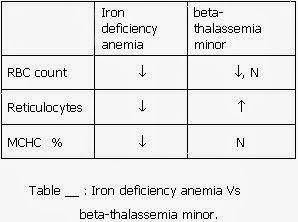
Careful analysis of the hemogram from patients with iron deficiency anemia and beta-thalassemia minor also provides sufficient information to favor one or the other diagnosis in many instances. For comparative analysis, the two hemograms are listed in tables below.
There are certain numerical differences which many a times are helpful in making this distinction. These are listed in table below.
Since iron deficiency anemia is associated with suppression of δ chain synthesis, Hb A2 in iron deficiency anemia is decreased. If a patient has beta-thalassemia minor as well as iron deficiency anemia, the level of hemoglobin A2 may be normal or even below normal. This is because the two diseases have an opposite effect on Hb A2 level. Diagnosis of beta-thalassemia minor in this scenario is likely to be missed. It is therefore mandatory that iron deficiency be corrected with iron therapy for 6-8 weeks and Hb A2 be re-estimated after iron deficiency has been corrected. An increase in the level of Hb A2 after iron therapy indicates an associated β Thalassaemia minor.
Hb A2 can be estimated by elution method, by densitometery and by column chromatography. Of these three methods, column chromatography seems to be a better discriminator. If Hb A2 level as determined by densitometery does not conform to the clinical status of the patient, it should be re-checked with chromatographic technique.
Age : 24 Sex: Female Occupation: Housewife
NUMERICAL VALUES
Beta – Thalassaemia Minor
Beta-thalassemia minor is a genetic disorder which shows strong geographical predilection. It is mostly encountered along the Mediterranean belt, the Arabian Peninsula and the Indo-Pak subcontinent. In Pakistan the frequency of beta-thalassemia gene is nearly 6 %. It is therefore not uncommon to come across these patients in clinical practice. A systematic analysis of the hemogram highlights the following features.
NUMERICAL:
Hemoglobin and hematocrit are both decreased. An unexpected finding is a high red cell count. In addition, the reticulocyte count is also increased. Total leukocyte count, platelet count and ESR are within normal limits.
RED CELL INDICES:
MCV and MCH are significantly decreased while MCHC% is nearly normal. This is at variance with the expected value of MCHC% which is decreased in almost all instances where MCV and MCH are below normal as exemplified by iron deficiency anemia. Red cells are microcytic and hypochromic hence anemia is of microcytic and hypochromic type.
DIFFERENTIAL LEUKOCYTE COUNT:
There is no deviation from the norm in the percentage values of different types of white cells. No abnormal leukocytes are seen.
MORPHOLOGY:
As expected, the morphology of the peripheral blood smear is quite revealing. The abnormalities are confined almost entirely to the red cell series. There is some variation in the size and shape of the red cells which, in conformity with the red cell indices, are predominantly microcytic and ‘hypochromic’. In addition some fragmented red cells, pencil cells and micro-spherocytes are also seen. A prominent feature is the presence of target cells and stippled red cells (basophilic stippling). There is also some variation in the color of the erythrocytes. Many hypochromic, some normochromic, a few polychromatophilic and occasional brightly stained red cells are present. This tinctorial heterogeneity is called anisochromia or anisochromasia.
Polychromatophilic erythrocytes are a shade larger than the normochromic red cells and on reticulocyte stain they display the characteristic reticulum in their cytoplasm. Polychromasia on Romanowsky’s stains (Wright’s, Leishman’s or Giemsa’s stain) is the counterpart of the reticulocytes on reticulocyte stain ; the greater the polychromasia, the higher the reticulocyte count.
Microcytic and hypochromic red cells are seen in a number of conditions; these are listed below.
• Iron deficiency anemia
• Thalassaemia syndromes
• Hemoglobinopathies
• Sideroblastic anemias
• Chronic lead toxicity
• Chronic renal failure
• Chronic infections
Of these disorders, iron deficiency anemia and Thalassaemia syndromes account for almost 90% of the cases of significant microcytosis and hypochromia (MCV less than 70 fl and MCH less than 25 pg).
A detailed history and a thorough physical examination coupled with socio-economic, obstetric and family history can help identify these two conditions in a vast majority of cases.
Careful analysis of the hemogram from patients with iron deficiency anemia and beta-thalassemia minor also provides sufficient information to favor one or the other diagnosis in many instances. For comparative analysis, the two hemograms are listed in tables below.
There are certain numerical differences which many a times are helpful in making this distinction. These are listed in table below.
Since iron deficiency anemia is associated with suppression of δ chain synthesis, Hb A2 in iron deficiency anemia is decreased. If a patient has beta-thalassemia minor as well as iron deficiency anemia, the level of hemoglobin A2 may be normal or even below normal. This is because the two diseases have an opposite effect on Hb A2 level. Diagnosis of beta-thalassemia minor in this scenario is likely to be missed. It is therefore mandatory that iron deficiency be corrected with iron therapy for 6-8 weeks and Hb A2 be re-estimated after iron deficiency has been corrected. An increase in the level of Hb A2 after iron therapy indicates an associated β Thalassaemia minor.
Hb A2 can be estimated by elution method, by densitometery and by column chromatography. Of these three methods, column chromatography seems to be a better discriminator. If Hb A2 level as determined by densitometery does not conform to the clinical status of the patient, it should be re-checked with chromatographic technique.





0 comments:
Post a Comment